Ehr Imrpove Continuity of Care in Urgent Care
 Guest post written by multiple neurosurgeons and neurosurgical residents from Stanford University Medical Center .
Guest post written by multiple neurosurgeons and neurosurgical residents from Stanford University Medical Center .
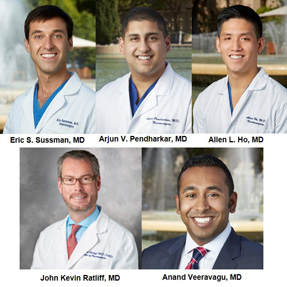
Eric S. Sussman , MD, Neurosurgery Resident; Arjun V. Pendharkar , MD, Neurosurgery Resident; Allen L. Ho , MD, Neurosurgery Resident; Anand Veeravagu , MD, Assistant Professor of Neurosurgery, Assistant Professor Orthopedic Surgery and Director of Minimally Invasive NeuroSpine Surgery; and John K. Ratliff , MD, FAANS, FACS, Professor and Vice Chair of Neurosurgery, Departmental Quality Officer and Co-Director of the Spine and Peripheral Nerve Surgery Division.
Imagine this common scenario: A critically ill neurosurgery patient requires transfer to a tertiary hospital. On arrival, the on-call neurosurgery resident has a formidable task ahead. The patient requires evaluation and stabilization, initiation of treatments and interventions, review of outside hospital records, and preparation for possible emergent neurosurgical intervention. In theory, the widespread implementation of electronic health records (EHRs) should streamline and facilitate these tasks. In reality, EHRs more often complicates things and thus negatively impacts patient care.
 Today, different hospitals and physician practices overwhelmingly utilize EHRs that cannot communicate with one another. For example, a transferred patient arrives with an unwieldy printout from the transferring facility. The superfluous medical documentation facilitated (and sometimes mandated) by EHRs result in records that are often overflowing with immaterial and redundant data; thus obscuring the acutely relevant data. To provide optimal emergent care to the transferred patient, the receiving physician team is often forced to duplicate the diagnostic workup resulting in lost time and unnecessary cost. Given the extensive regulatory requirements related to EHRs, how is this possible? To understand, we must first turn the clock back.
Today, different hospitals and physician practices overwhelmingly utilize EHRs that cannot communicate with one another. For example, a transferred patient arrives with an unwieldy printout from the transferring facility. The superfluous medical documentation facilitated (and sometimes mandated) by EHRs result in records that are often overflowing with immaterial and redundant data; thus obscuring the acutely relevant data. To provide optimal emergent care to the transferred patient, the receiving physician team is often forced to duplicate the diagnostic workup resulting in lost time and unnecessary cost. Given the extensive regulatory requirements related to EHRs, how is this possible? To understand, we must first turn the clock back.
Before 2014, despite the anticipated benefits, adoption of EHR was slow. Then the American Recovery and Reinvestment Act required that all health care providers adopt and demonstrate meaningful use of EHRs by Jan. 1, 2014. Because of this increased demand for EHRs, many new health information technology (IT) software systems have been developed and implemented at health care facilities throughout the United States. By the end of 2016, more than 95 percent of hospitals and 60 percent of office-based health care organizations had adopted EHRs in a "meaningful" capacity.
Beyond widespread adoption of EHR systems, one of the primary objectives of the EHR regulatory mandate was to improve data exchange and interconnectivity. EHRs have undoubtedly had a positive impact on some aspects of health care delivery; however, enhanced interconnectivity has yet to be realized. A recent Health Affairs report found that less than one-third of hospitals engage in finding, sending, receiving and integrating electronic patient information from outside hospitals. Furthermore, less than 20 percent used this data for direct patient care purposes. These numbers are staggering, particularly considering that just ten health IT companies account for more than 70 percent of licensed EHRs nationwide. In fact, data exchange is limited even between health care facilities that utilize the same EHR system.
Within Stanford's health care system, two different hospitals — Stanford Health Care (SHC) and Lucile Packard Children's Hospital (LPCH) — both utilize the same EHR (Epic). Despite being adjacent facilities on the same campus of Stanford University Medical Center, these hospitals have implemented independent Epic systems. The result is a logistical challenge for health care providers functioning in both hospitals simultaneously:
- Time-consuming login processes required to switch from the electronic health record of a pediatric patient to that of an adult patient.
- Barriers to the seamless continuity of patient care between the two closely inter-related facilities.
- Failure of merged EHRs when patients require movement between both hospitals. For example, a pediatric patient transported to the adult hospital (SHC) for a specialized procedure (e.g., neuro-interventional therapy or a nuclear medicine study) cannot have the procedural documentation in the same Epic EHR with the remainder of the clinical documentation of the hospitalization.
These issues are even more pronounced for patients who are transferred from a wholly different health care facility, which is a common occurrence. The transfer of care of such a critically ill patient becomes dependent on verbal communication and the unwieldy printed copy of the patient's medical record that accompanies the patient. Even more frustrating, after arrival, there is no seamless way with which to integrate the outside hospital's data into the accepting facility's EHR. This leads to both:
- Duplication of basic laboratory and diagnostic tests at the accepting facility (to facilitate emergent and urgent interventions or for medicolegal reasons); and
- Disruption of continuous trends in critical data including vital signs, laboratory tests, clinical assessments and medications.
One of the specific problems EHRs were supposed to address was facilitating this seamless transfer of legible and accurate information, to make health care professionals less reliant on hard to read or verbal communications. The inability of accepting providers to view diagnostic imaging before transfer further complicates these tenuous transitions of care.
Some aspects of recent regulatory activity seek to answer this deficiency. For example, language in the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) and the 21st Century Cures Act call for achieving interoperability between different EHR systems. In our experience, however, this is far from realized. Different EHRs remain islands of data, unable to talk to each other and unable to achieve their primary goal: capturing and sharing patient health information to improve the quality of care provided.
Care Everywhere is a health information exchange platform within Epic's EHR system intended to facilitate interconnectivity between health care facilities. This is potentially a giant leap forward with respect to facilitating seamless patient care between various health care institutions. Nonetheless, this platform has limited availability, and the interface is not yet seamlessly integrated with the remainder of the patient's EHR. Also, this platform does not yet support the transfer of radiographic imaging between facilities.
Separate regulatory requirements and previous iterations of the meaningful use program (formerly part of the EHR Incentive Programs), has been deemed "meaningless use" by most physicians because it's another source of frustration. A RAND Corporation report commissioned by the American Medical Association (AMA) focused on physician professional satisfaction found EHRs and meaningful use regulations were major sources of practice frustration. While physicians supported the goals of EHR adoption — improving care through facilitating communication and improving medical record maintenance — in execution "meaningless use" was a tremendous headache. Redundant data entry, repetitive documentation, and lack of flexibility in documentation requirements made compliance a challenge. Physicians found themselves repetitively jumping through documentation hoops, with less face time devoted to patient care and more screen time devoted to checking boxes to fulfill regulatory requirements. This has improved with transition from "meaningless use" to the Advancing Care Information aspect of MACRA's Quality Payment Program (QPP). However, the new system still suffers from lack of flexibility, with many performance metrics relevant only to select practices and physicians.
The universal transition to EHRs holds excellent potential for improving the quality and continuity of patient care in our complex health care system. Regulatory demands should be designed to ensure that real quality and functionality are promoted. Unfortunately, almost four years after the government-mandated transition deadline, EHRs are still plagued by a lack of interconnectivity between health care practices and facilities. Immediate efforts should be undertaken to establish a seamless platform for data exchange and to universal compatibility of EHR systems.
Editor's Note: We encourage everyone to join the conversation online by using the hashtag #RegRelief.
Source: https://www.neurosurgeryblog.org/2017/12/15/ehr-interconnectivity-challenges-continue-to-impact-patient-care/
0 Response to "Ehr Imrpove Continuity of Care in Urgent Care"
Post a Comment